
Blog & Updates on Vancouver Prenatal Classes

The Postpartum Waterfall: Tips to Survive Newborn Hell
Baby’s needs are simple, but they are all-the-time. It’s like having to keep a balloon in the air: it doesn’t require any particular skill, but you can’t do anything else at the same time.


The Terror Of Tearing: Demystifying The Dreaded ‘tearing’ During Birth
A very common fear before giving birth for the first time is the idea of tearing. And it’s obvious why. The image of having your body ripped open is dreadful and appalling. It’s terrifying. The very idea makes anyone cringe and cower, and gives the impression that birth will be excruciatingly painful, and damaging to your very bodily integrity.
But this particular image is somewhat misleading. It’s an inaccurate analogy that is based on centuries of not understanding everything that happens during birth, and focusing exclusively on the idea of the mechanics of one body bursting out of another. Yes, that sounds scary, like the movie Alien, or The Substance, or countless other iconic images of parasitic host-body horror. But this is not a good metaphor for birth, because it misses all the quiet ways our body can help us birth the baby, and stay intact while doing so.
Here are twelve facts about your perineum that might change the way you think about a baby emerging from your body.
Do You Need a Doula? 8 Reasons Why You Do
Do you need a doula?
Yes you do!
Your birth will be better with a doula. Any birth will be better with a doula. Here are some of the reasons.
Cervical Dilation: 12 Fun Facts
Almost everyone knows that one important aspect of labour is that the cervix has to dilate from zero to ten centimetres. But what does this actually mean? What is the cervix, how does it dilate, and how does that relate to your birth? And more importantly, does it hurt? Here are twelve things you might not know about the cervix and dilation.

Neuroception
Babies are born with the superpower to detect danger in their surroundings, and this same superpower helps with long-term brain development. What is it? Neuroception.
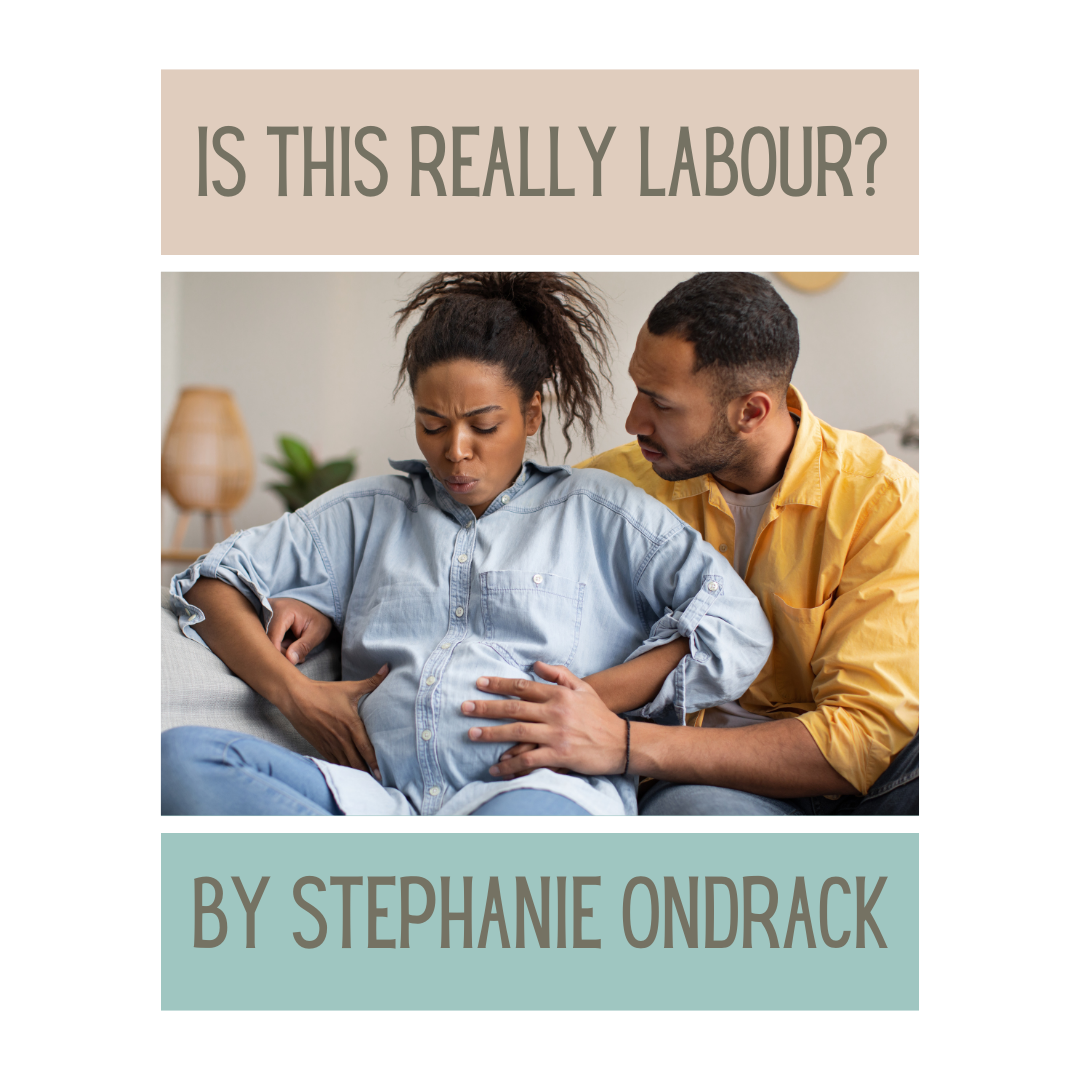
Is This Really Labour?
Recognising the signs of labour can be an elusive and vague target. Until you’re actually in it. Then it’s pretty unmistakable. But only if you know what you’re looking for.
So what are the signs of actual labour?
First, let’s start with what’s not.

Drinking in Labour
Why is hydration so beneficial during childbirth? Read our latest blog post to find our why.
As Smooth as a Baby’s Bottom: Everything You Never Wanted to Know About Diaper Rash
You’ve heard the expression, ‘as smooth as a baby’s bottom’? A baby’s bottom is indeed supposed to be smooth, healthy, and perfect. But often our poor little ones are afflicted with unhappy, irritated skin in the diaper area. So what can we do to prevent this, and if it happens anyway, what can we do to help?
Pregnancy Dreams
Are you having crazy dreams during your pregnancy? You’re not alone. Pregnancy affects our whole body, all our systems, floods us with new hormones, and even changes our senses. Is it any wonder it also affects our minds?
Preparing for a Caesarean Birth: TEN THINGS YOU CAN DO
If you have a scheduled Caesarean, or if you end up needing an unplanned one, there are several things you can do to improve the experience. Here are ten things you can do.
